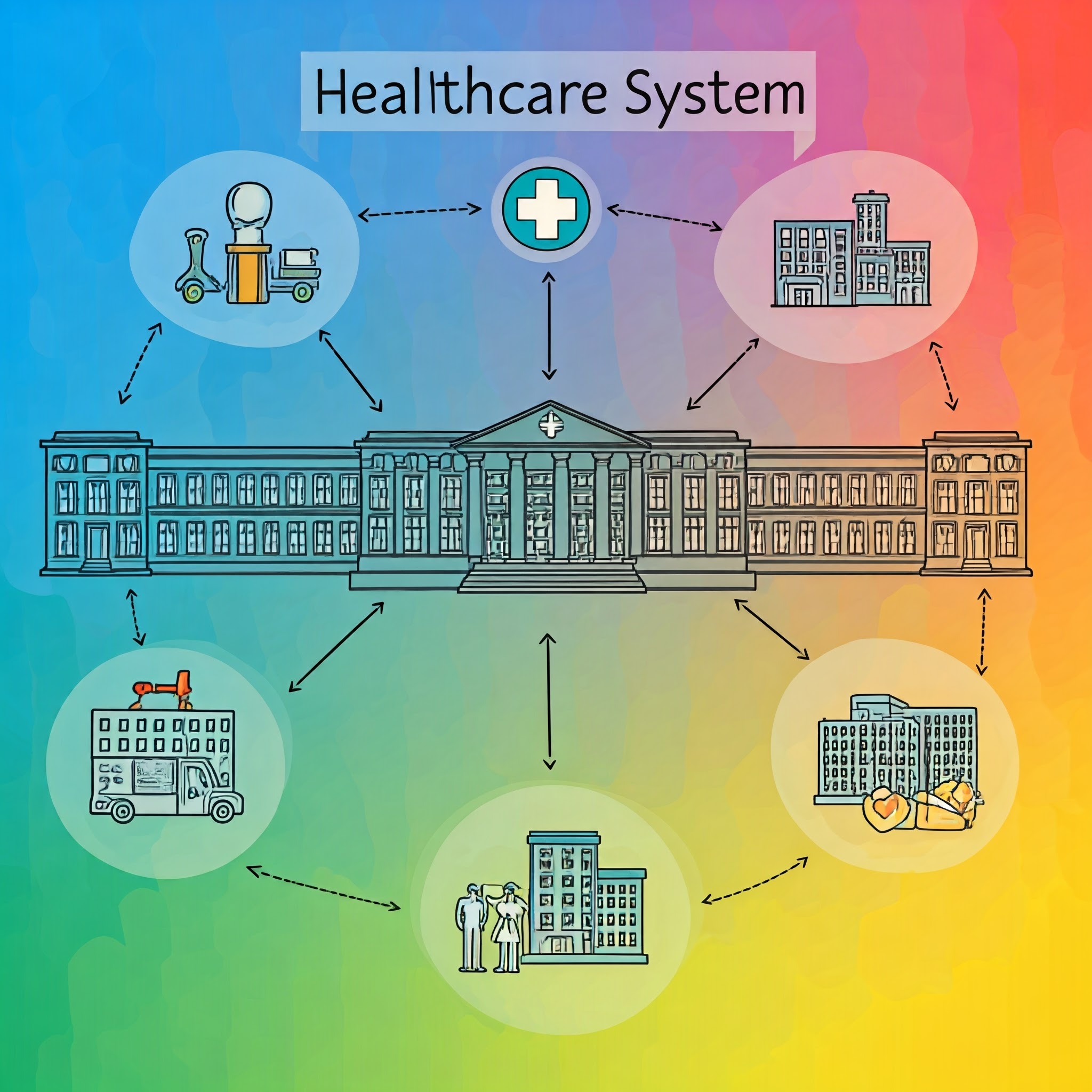
The United States healthcare delivery system represents one of the most complex and multifaceted organizational structures in modern healthcare. According to the Centers for Medicare & Medicaid Services, healthcare spending reached a remarkable $4.3 trillion in recent years, emphasizing the scale and significance of this system. This comprehensive analysis provides a detailed examination of the intricate networks, relationships, and mechanisms that comprise healthcare delivery in the United States, utilizing visual representations to illuminate complex concepts and relationships.
The Shared Responsibility for Health Care
The United States healthcare system operates through a complex framework of shared responsibilities distributed across federal, state, and local governmental entities. This multi-tiered approach creates a comprehensive structure for healthcare delivery while allowing for both standardization and regional adaptation of healthcare services.
Federal Level Oversight and Administration
The federal government establishes fundamental healthcare policies and regulations that form the foundation of the nation’s healthcare system. Through key agencies such as the Department of Health and Human Services (HHS), Centers for Medicare & Medicaid Services (CMS), and the Centers for Disease Control and Prevention (CDC), the federal government implements and oversees critical healthcare initiatives. These organizations manage essential programs serving millions of Americans, including Medicare, which provides health coverage to approximately 65 million beneficiaries.
Key federal responsibilities include:
- Establishing national healthcare policies and regulations
- Administering Medicare and partnering with states on Medicaid
- Funding medical research through the National Institutes of Health
- Implementing nationwide health initiatives and programs
- Enforcing healthcare quality standards and safety regulations
- Tax policies favorable to employer health insurance
- Fund physician training
State-Level Implementation and Oversight
State governments serve as crucial intermediaries in the healthcare delivery system, adapting federal guidelines while implementing state-specific programs. States maintain significant autonomy in healthcare administration, allowing them to tailor programs to their populations’ unique needs while adhering to federal requirements.
Primary state healthcare responsibilities encompass:
- Administering and funding state Medicaid programs
- Licensing and regulating healthcare facilities and professionals
- Operating state health departments
- Managing health insurance marketplaces
- Developing state-specific healthcare regulations
- Implementing public health programs
- Care provisions including operation of facilities for mentally ill
Local Government Healthcare Delivery
Local government entities function as direct service providers, implementing healthcare initiatives at the community level. These organizations play a vital role in addressing immediate public health needs and ensuring healthcare accessibility within their jurisdictions.
Essential local healthcare functions include:
- Operating community health clinics and facilities
- Managing emergency medical services
- Conducting health inspections and enforcement
- Monitoring community health trends
- Coordinating local healthcare resources
- Developing and enforcing public health codes
Collaborative Healthcare Delivery
The effectiveness of the U.S. healthcare system depends significantly on the coordinated efforts across all three governmental levels. This collaboration enables:
- Comprehensive healthcare coverage across populations
- Efficient resource allocation and utilization
- Standardized quality measures and outcomes
- Adaptable healthcare delivery models
- Responsive public health initiatives
Through this multi-tiered approach, the healthcare system can maintain consistent national standards while accommodating regional variations and specific community needs. The framework allows for innovation in healthcare delivery methods while ensuring adherence to established quality and safety protocols.
Understanding this shared responsibility model is crucial for healthcare administrators, policymakers, and providers working to optimize healthcare delivery and improve population health outcomes. The system’s success relies on effective coordination, clear communication channels, and strategic alignment of objectives across all governmental levels.

Source: Adopted from Health Care Delivery in the United States, p 14.
Significant health policy milestones
The evolution of U.S. healthcare policy represents a series of transformative legislative actions that have fundamentally reshaped the healthcare delivery landscape. These milestone policies have progressively expanded healthcare access, enhanced patient protections, and modernized healthcare delivery systems across the nation.
Medicare and Medicaid Establishment (1965)
The Social Security Amendments of 1965 marked a watershed moment in U.S. healthcare policy through the creation of Medicare and Medicaid. Medicare established comprehensive health coverage for Americans aged 65 and older, while Medicaid provided healthcare access for low-income individuals and families. This legislation represented the largest expansion of healthcare coverage in U.S. history to that point, with Medicare initially enrolling 19 million beneficiaries.
Key implementations included:
- Hospital insurance (Part A) for inpatient services
- Medical insurance (Part B) for outpatient care
- State-administered Medicaid programs
- Standardized healthcare coverage requirements
COBRA Implementation (1986)
The Consolidated Omnibus Budget Reconciliation Act (COBRA) introduced crucial protections for employees facing potential loss of health insurance coverage. This legislation mandated that employers with 20 or more employees must offer continued health coverage to qualifying individuals for up to 18 months following employment termination.
COBRA provisions established:
- Temporary continuation of group health coverage
- Protection for employees and their dependents
- Standardized notification requirements
- Premium payment frameworks
Children’s Health Insurance Programs (CHIPs) (1996)
The Children’s Health Insurance Program (CHIP) represents a pivotal component of the U.S. healthcare safety net, designed specifically to bridge the coverage gap for children in moderate-income families. This federal-state partnership program provides comprehensive health coverage to children whose families earn too much to qualify for Medicaid but cannot afford private insurance.
Program achievements include:
- Extended coverage to over 9 million children
- State-administered program flexibility
- Comprehensive pediatric health benefits
- Cost-sharing provisions with states
HIPAA Enactment (1997)
The Health Insurance Portability and Accountability Act established foundational standards for healthcare information privacy and security. This legislation created comprehensive frameworks for protecting patient data while facilitating necessary information sharing among healthcare providers.
Critical HIPAA components:
- Patient privacy protections
- Security standards for health information
- Insurance coverage portability
- Administrative simplification requirements
Medicare Prescription Drug Coverage (2003)
The Medicare Modernization Act introduced Part D prescription drug coverage, addressing a significant gap in Medicare benefits. This expansion represented the largest overhaul of Medicare since its inception, providing essential medication coverage for millions of beneficiaries.
Key provisions included:
- Voluntary prescription drug benefits
- Private plan administration options
- Income-based premium subsidies
- Coverage gap (“donut hole”) provisions
Affordable Care Act Implementation (2010)
The Patient Protection and Affordable Care Act introduced comprehensive healthcare reforms, fundamentally altering the U.S. healthcare landscape. This legislation implemented sweeping changes to expand coverage, enhance consumer protections, and improve healthcare quality.
Transformative elements encompassed:
- Individual coverage mandate
- Health insurance marketplace establishment
- Essential health benefits requirements
- Medicaid expansion provisions
- Pre-existing condition protections
These milestone policies collectively demonstrate the progressive development of U.S. healthcare policy, each building upon previous legislation to create more comprehensive healthcare coverage and enhanced patient protections. Understanding these developments is crucial for healthcare administrators, policymakers, and providers as they continue to shape and implement healthcare delivery systems.
H2: A Comparative Perspective
The analysis of healthcare systems across developed nations reveals significant variations in funding mechanisms, expenditure patterns, and health outcomes. Understanding these differences provides crucial insights into the effectiveness and efficiency of different healthcare delivery models.
Sources and Uses of Healthcare Funding
Healthcare financing varies substantially across developed nations, reflecting different philosophical approaches to healthcare delivery:
United States:
- Multiple funding sources including private insurance
- Government programs (Medicare/Medicaid)
- Out-of-pocket payments
- Other private sources
European Union:
- Predominantly public funding through taxation
- Universal coverage models
- Supplementary private insurance
- Minimal out-of-pocket expenses
- Social insurance systems
Asian Models (Japan/South Korea):
- Universal health insurance systems
- Employer-based contributions
- Government subsidies
- Regulated fee structures
Healthcare Spending Patterns
Global healthcare expenditure patterns reveal striking disparities:
United States:
- Highest per capita spending
- 18.3% of GDP devoted to healthcare
- Significantly higher administrative costs
- Higher pharmaceutical pricing
- Advanced technology investments
OECD Countries (Average):
- Per capita spending ($4,000-6,000 annually)
- 8.8% – 11.2% of GDP
- Lower administrative overhead
- Regulated drug pricing
- Controlled technology acquisition
Life Expectancy and Health Outcomes
Despite higher spending, health outcomes show notable variations:
Life Expectancy Comparisons:
- Japan: 84.7 years
- Switzerland: 83.8 years
- Australia: 83.2 years
- European Union average: 81.3 years
- United States: 77.8 years
Contributing Factors:
- Access to preventive care
- Lifestyle and dietary patterns
- Environmental conditions
- Social determinants of health
- Healthcare system efficiency
Healthcare system design can significantly impacts both efficiency and outcomes. Countries with unified funding mechanisms and universal coverage generally achieve better population health outcomes despite lower per-capita spending. The U.S. system, while offering advanced care options and rapid access to specialists, shows higher costs and lower overall population health metrics compared to other developed nations.
Healthcare workforce
The healthcare workforce represents a complex network of professionals operating across various care settings, each requiring specific skillsets and certifications to meet diverse patient needs. Understanding the distribution and roles of healthcare workers across different care environments is crucial for effective healthcare delivery.
Inpatient Care Workforce
Hospital-based care requires a comprehensive team of healthcare professionals operating in a 24/7 environment:
Clinical Staff:
- Physicians (hospitalists, specialists)
- Registered nurses (RNs)
- Licensed practical nurses (LPNs)
- Certified nursing assistants (CNAs)
- Respiratory therapists
- Physical/occupational therapists
- Clinical laboratory technicians
- Radiologic technologists
Support Personnel:
- Unit coordinators/clerks
- Environmental services staff
- Nutritional services workers
- Materials management staff
- Security personnel
- Information technology specialists
Administrative Staff:
- Hospital administrators
- Department managers
- Clinical coordinators
- Quality improvement specialists
- Medical records personnel
Ambulatory Care Workforce
Outpatient settings require professionals focused on preventive care and chronic disease management:
Primary Care Providers:
- Family physicians
- Internal medicine specialists
- Pediatricians
- Nurse practitioners
- Physician assistants
- Medical assistants
Specialty Care Providers:
- Medical specialists
- Surgical specialists
- Diagnostic technicians
- Outpatient nurses
- Physical therapists
- Occupational therapists
- Mental health professionals
Support Staff:
- Practice managers
- Medical receptionists
- Billing specialists
- Scheduling coordinators
- Quality assurance personnel
- Care coordinators
Long-Term Care Workforce
Long-term care facilities require staff specialized in geriatric and chronic care management:
Direct Care Providers:
- Registered nurses
- Licensed practical nurses
- Certified nursing assistants
- Patient care technicians
- Rehabilitation specialists
- Social workers
- Activities directors
Specialized Support:
- Geriatric care managers
- Dietitians
- Mental health specialists
- Hospice care providers
- Respiratory therapists
- Wound care specialists
Administrative Personnel:
- Facility administrators
- Director of nursing
- Quality assurance coordinators
- Medical records staff
- Human resources personnel
- Financial managers

Source: Adopted from Health Care Delivery in the United States, p 22.
Workforce Challenges and Trends
Current issues affecting the healthcare workforce include:
Staffing Challenges:
- Ongoing nursing shortages
- Geographic maldistribution
- High turnover rates
- Burnout prevention
- Competitive recruitment
Educational Requirements:
- Continuing education needs
- Certification maintenance
- Skill updates for new technologies
- Cross-training requirements
- Specialization demands
Emerging Workforce Trends:
- Telehealth competencies
- Digital health integration
- Team-based care models
- Cultural competency requirements
- Population health management
Future Workforce Considerations:
- Aging workforce demographics
- Increasing demand for services
- Technology integration needs
- Changing care delivery models
- Evolving skill requirements
The healthcare workforce continues to evolve in response to changing patient needs, technological advancements, and healthcare delivery models. Understanding these dynamics is essential for healthcare organizations to maintain adequate staffing levels and ensure quality care delivery across all settings.
Variations in healthcare delivery
Healthcare delivery in the United States exhibits significant variations across geographic regions, populations, and delivery systems. These variations manifest in quality metrics, cost structures, and access to care, creating a complex landscape that healthcare administrators and policymakers must navigate to improve system efficiency and effectiveness.
Healthcare Quality Variations Across the Nation
Quality variations in healthcare delivery represent one of the most pressing challenges in the U.S. healthcare system. Studies consistently demonstrate substantial differences in healthcare quality across regions, often independent of population characteristics or resource availability. These variations appear in mortality rates, hospital readmissions, and patient outcomes, suggesting systemic differences in care delivery approaches.
The most significant quality variations often occur between urban and rural healthcare settings. Urban areas typically benefit from higher concentrations of specialists, advanced medical technologies, and research institutions. Conversely, rural areas face challenges in recruiting healthcare professionals, maintaining specialized services, and accessing cutting-edge treatments. This disparity creates measurable differences in health outcomes for conditions ranging from chronic disease management to acute care interventions.
Socioeconomic factors further compound these quality variations. Communities with higher poverty rates and limited healthcare access often experience poorer health outcomes, higher rates of preventable hospitalizations, and increased mortality rates for manageable conditions. These disparities persist despite numerous policy initiatives aimed at equalizing healthcare quality across populations.
Healthcare Costs and Value Analysis
Healthcare costs demonstrate remarkable variation across different regions of the United States, with some areas spending up to three times more per capita than others without corresponding improvements in outcomes. These cost variations reflect differences in practice patterns, resource utilization, and market dynamics rather than population health needs or quality of care delivered.
Several factors contribute to regional cost variations. Provider concentration in certain markets can lead to higher prices through reduced competition. Practice pattern variations result in different utilization rates for procedures and services, while local labor markets affect workforce costs. Administrative overhead and regulatory compliance requirements also vary significantly by region, contributing to cost disparities.
The relationship between healthcare costs and value remains complex. Higher-cost regions do not consistently demonstrate better outcomes, suggesting opportunities for efficiency improvements. Value-based care initiatives attempt to address this disconnect by linking reimbursement to quality metrics and patient outcomes rather than service volume.
The Future of Healthcare Delivery
The evolution of healthcare delivery systems continues to accelerate, driven by technological innovations, changing patient expectations, and economic pressures. Telehealth expansion represents one of the most significant shifts in care delivery, enabling remote consultations, monitoring, and treatment management. This technology-enabled care model promises to reduce access barriers while potentially lowering delivery costs.
Artificial intelligence and machine learning applications are increasingly integrated into clinical decision support systems, diagnostic processes, and administrative functions. These technologies offer opportunities to improve diagnostic accuracy, predict patient risks, and optimize resource allocation. However, their implementation requires careful consideration of ethical implications and equity concerns. Population health management approaches are gaining prominence as healthcare organizations seek to improve outcomes while controlling costs. These strategies emphasize preventive care, chronic disease management, and community health initiatives. Success in population health management requires sophisticated data analytics, care coordination capabilities, and engaged patient populations.
Value-based care models continue to evolve, moving away from traditional fee-for-service arrangements toward payment systems that reward quality and efficiency. These models encourage provider organizations to focus on outcomes rather than service volume, potentially reducing unnecessary procedures and improving care coordination.
Integration of social determinants of health into care delivery represents another significant trend. Healthcare organizations increasingly recognize that factors such as housing, nutrition, and social support significantly impact health outcomes. This understanding leads to expanded partnerships with community organizations and social service providers.
Digital health platforms are becoming central to healthcare delivery, offering patients greater access to their health information, communication with providers, and self-management tools. These platforms facilitate care coordination, reduce administrative burden, and enable more personalized care approaches.
Looking forward, healthcare delivery systems must balance innovation with accessibility and equity. While technological advances offer tremendous potential for improving care delivery, ensuring these benefits reach all populations remains a critical challenge. Success requires thoughtful policy development, sustainable funding mechanisms, and committed leadership from healthcare organizations.
The transformation of healthcare delivery systems continues to accelerate, driven by the need to address current variations while preparing for future challenges. Organizations that successfully navigate these changes will likely demonstrate strong capabilities in technology adoption, workforce development, and patient engagement while maintaining focus on quality improvement and cost management.
References:
Knickman, J., & Elbel, B. (2019). Jonas & Kovner’s health care delivery in the United States (12th ed.). Springer Publishing Company.